Abstract
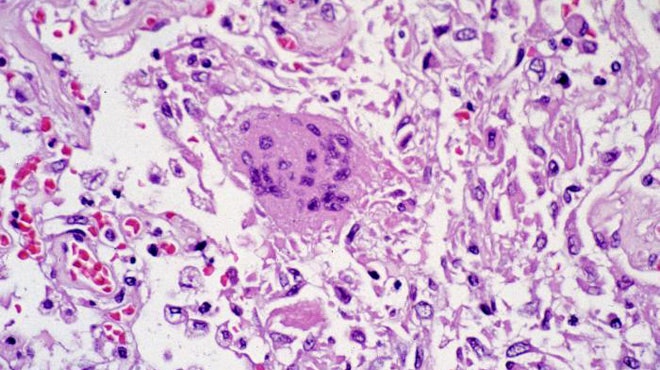
The SARS-CoV-2 virus causing COVID-19 pandemic across the world has highlighted the risk of human-to-human transmission, the speed of spread in a globally mobile population and the need for health services to be flexible in their responses to hitherto unknown challenges. One of the hallmarks of COVID-19 is severe acute respiratory syndrome presenting with widespread viral pneumonitis and respiratory failure. It is therefore not unusual for patients with chronic lung diseases such as asthma, COPD, and bronchiectasis to be concerned regarding their particular vulnerability. As healthcare professionals responsible for the care of such patients, it is important to understand how the SARS-CoV-2 virus impacts the respiratory system and the outcomes for patients with chronic lung disease. This review examines the evidence and offers sensible guidance until more is known.
References
Peer reviewed by Simon Godwin MD FRCP, Basildon Hospital, Essex, UK
Zhang, J. et al. Clinical characteristics of 140 patients infected with SARS‐CoV‐2 in Wuhan, China. Allergy https://onlinelibrary.wiley.com/doi/abs/10.1111/all.14238 (2020).
Hageman, J. R. The Coronavirus Disease 2019 (COVID-19). Pediatr. Ann. 49, e99–e100 (2020).
Zhang, T., Wu, Q. & Zhang, Z. Probable Pangolin Origin of SARS-CoV-2 Associated with the COVID-19 Outbreak. Curr. Biol. 0, (2020).
Qu, G., Li, X., Hu, L. & Jiang, G. An Imperative Need for Research on the Role of Environmental Factors in Transmission of Novel Coronavirus (COVID-19). Environ. Sci. Technol. (2020) doi:10.1021/acs.est.0c01102.
Wu, Y.-H. et al. Pulmonary IL-33 orchestrates innate immune cells to mediate RSV-evoked airway hyperreactivity and eosinophilia. Allergy n/a,.
Gavala, M. L., Bashir, H. & Gern, J. E. Virus/Allergen Interactions in Asthma. Curr. Allergy Asthma Rep. 13, 298–307 (2013).
Kurai, D., Saraya, T., Ishii, H. & Takizawa, H. Virus-induced exacerbations in asthma and COPD. Front. Microbiol. 4, (2013).
Lupia, T. et al. 2019 novel coronavirus (2019-nCoV) outbreak: A new challenge. J. Glob. Antimicrob. Resist. 21, 22–27 (2020).
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet 395, 497–506 (2020).
Chen, N. et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. The Lancet 395, 507–513 (2020).
McManus, T. E. et al. Respiratory viral infection in exacerbations of COPD. Respir. Med. 102, 1575–1580 (2008).
Monto, A. S. Epidemiology of Respiratory Viruses in Persons with and without Asthma and COPD. Am. J. Respir. Crit. Care Med. 151, 1653–1658 (1995).
Gorse, G. J., O’Connor, T. Z., Hall, S. L., Vitale, J. N. & Nichol, K. L. Human Coronavirus and Acute Respiratory Illness in Older Adults with Chronic Obstructive Pulmonary Disease. J. Infect. Dis. 199, 847–857 (2009).
Frickmann, H. et al. The influence of virus infections on the course of COPD. Eur. J. Microbiol. Immunol. 2, 176–185 (2012).
Johnston, S. L. Overview of Virus-induced Airway Disease. Proc. Am. Thorac. Soc. 2, 150–156 (2005).
Belouzard, S., Millet, J. K., Licitra, B. N. & Whittaker, G. R. Mechanisms of coronavirus cell entry mediated by the viral spike protein. Viruses 4, 1011–1033 (2012).
Li, W. et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature 426, 450–454 (2003).
Zhang, Y. et al. Upregulation of Angiotensin (1-7)-Mediated Signaling Preserves Endothelial Function Through Reducing Oxidative Stress in Diabetes. Antioxid. Redox Signal. 23, 880–892 (2015).
McCarthy, M. Texas healthcare worker is diagnosed with Ebola. BMJ 349, (2014).
Judson, S. D. & Munster, V. J. Nosocomial Transmission of Emerging Viruses via Aerosol-Generating Medical Procedures. Viruses 11, (2019).
van Doremalen, N. et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 0, null (2020).
Thomas, R. J. Particle size and pathogenicity in the respiratory tract. Virulence 4, 847–858 (2013).
Tran, K., Cimon, K., Severn, M., Pessoa-Silva, C. L. & Conly, J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PloS One 7, e35797 (2012).
Raboud, J. et al. Risk factors for SARS transmission from patients requiring intubation: a multicentre investigation in Toronto, Canada. PloS One 5, e10717 (2010).
Wan, G.-H., Tsai, Y.-H., Wu, Y.-K. & Tsao, K.-C. A large-volume nebulizer would not be an infectious source for severe acute respiratory syndrome. Infect. Control Hosp. Epidemiol. 25, 1113–1115 (2004).
Booth, T. F. et al. Detection of airborne severe acute respiratory syndrome (SARS) coronavirus and environmental contamination in SARS outbreak units. J. Infect. Dis. 191, 1472–1477 (2005).
Public Health England. Guidance COVID-19 personal protective equipment (PPE). Available from: https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-personal-protective-equipment-ppe [Accessed 19th May 2020]
Seto, W. et al. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). The Lancet 361, 1519–1520 (2003).
World Health Organisation. Coronavirus disease (COVID-19) advice for the public. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public [Accessed 19th May 2020]
World Health Organisation. WHO Director-General’s opening remarks at the media briefing on COVID-19 - 16 March 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---16-march-2020 [Accessed 19th May 2020]
Zumla, A., Chan, J. F. W., Azhar, E. I., Hui, D. S. C. & Yuen, K.-Y. Coronaviruses — drug discovery and therapeutic options. Nat. Rev. Drug Discov. 15, 327–347 (2016).
Yuen, K.-S., Ye, Z.-W., Fung, S.-Y., Chan, C.-P. & Jin, D.-Y. SARS-CoV-2 and COVID-19: The most important research questions. Cell Biosci. 10, (2020).
Mehta, P. et al. COVID-19: consider cytokine storm syndromes and immunosuppression. The Lancet 395, 1033–1034 (2020).
Matthay, M. A., Aldrich, J. M. & Gotts, J. E. Treatment for severe acute respiratory distress syndrome from COVID-19. Lancet Respir. Med. 0, (2020).
Ni, Y.-N., Chen, G., Sun, J., Liang, B.-M. & Liang, Z.-A. The effect of corticosteroids on mortality of patients with influenza pneumonia: a systematic review and meta-analysis. Crit. Care Lond. Engl. 23, 99 (2019).
Woodhead, M. Inhaled Corticosteroids Cause Pneumonia …or Do They? Am. J. Respir. Crit. Care Med. 176, 111–112 (2007).
Kim, M. H. et al. Inhaled Corticosteroids in Asthma and the Risk of Pneumonia. Allergy Asthma Immunol. Res. 11, 795–805 (2019).
Molina, R. M. de et al. Inhaled corticosteroids and influenza A (H1N1) viral pneumonia. Eur. Respir. J. 40, (2012).
ICNARC – Latest news. https://www.icnarc.org/About/Latest-News/2020/04/04/Report-On-2249-Patients-Critically-Ill-With-Covid-19.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright (c) 2020 Array