Abstract
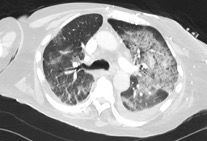
We report a case of a 61-year-old male who had recently been discharged home after contracting COVID-19 during an extended hospital admission. He presented to the emergency department after episode of sudden onset central chest pain and D-dimer was 390 mcg/L on admission. The patient was initially managed for acute coronary syndrome, however within twenty-four hours of admission the patient desaturated to 74% on room air and required 15L oxygen. CT Pulmonary Angiogram showed right lower lobe segmental pulmonary emboli and extensive COVID-19 lung changes. Subsequently, acute coronary syndrome treatment was stopped, and the patient treated for pulmonary embolus. Following this, his oxygen requirement improved significantly, and the patient stabilised within one week.
Emerging data and clinical evidence suggests an increased risk and prevalence of venous thromboembolic events in COVID-19, particularly in patients with more severe disease. It is currently unclear how long this increased risk persists. This case report highlights the importance of risk stratification of patients on discharge from hospital, to determine who requires extended thromboprophylaxis on discharge. Going forward, clinical trials are needed to evaluate the duration and dose of thromboprophylaxis in high-risk patients, and aid the formation of clearer guidelines for clinicians.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright (c) 2020 Array